Esophagus Cancer: What to Know, From Symptoms to Care
Esophagus cancer begins in the muscular tube that carries food from the throat to the stomach. While it’s less common than many other cancers, esophagus cancer can be aggressive if detected late. Knowing early warning signs, understanding risk factors, and getting timely diagnosis can make a meaningful difference. This guide explains common symptoms, how doctors diagnose and stage the disease, and current treatment options such as surgery, chemotherapy, radiation therapy, immunotherapy, and targeted therapy. It’s designed for general education and should not replace advice from your healthcare provider.
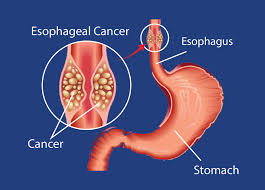
What Is Esophagus Cancer?
Esophagus cancer (often called esophageal cancer) develops when abnormal cells grow uncontrollably in the lining of the esophagus. The two main types are:
- Squamous cell carcinoma: usually forms in the upper or middle portions of the esophagus.
- Adenocarcinoma: often starts in glandular cells near the lower esophagus, frequently linked with chronic acid reflux and Barrett’s esophagus.
Signs & Symptoms
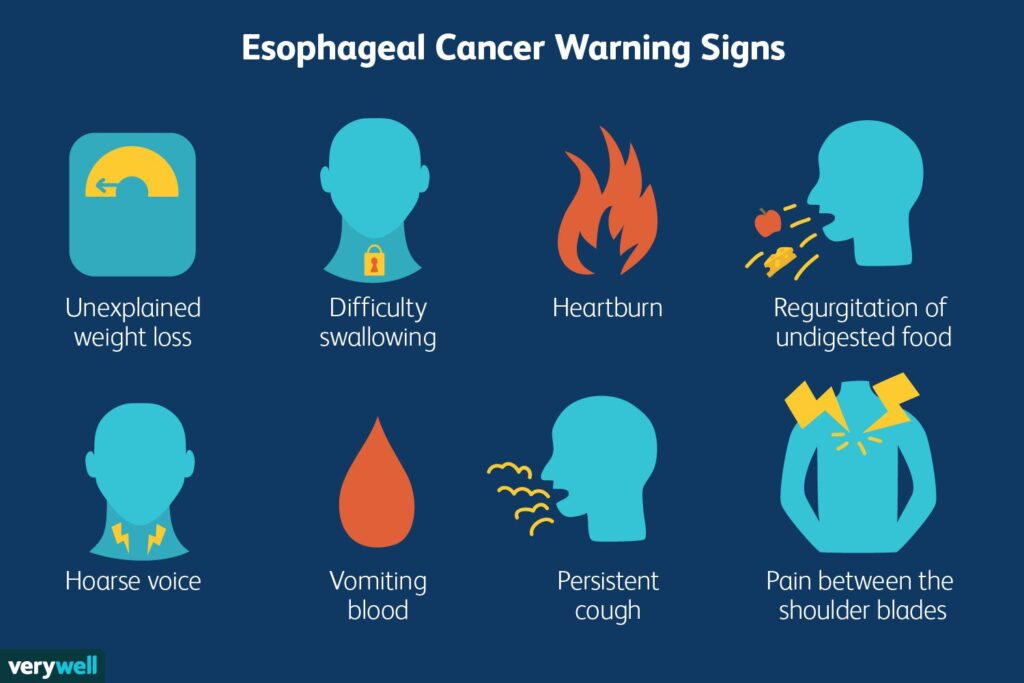
Early stages may cause few or no symptoms. As esophagus cancer advances, people may notice:
- Difficulty or pain when swallowing (dysphagia)
- Unintentional weight loss or poor appetite
- Chest discomfort or burning sensation
- Persistent cough or hoarseness
- Food regurgitation or a feeling of food “sticking”
- Ongoing heartburn or indigestion
Seek prompt medical evaluation if swallowing problems persist or worsen.
Risk Factors
Certain factors can increase the likelihood of esophagus cancer:
- Long-term tobacco use and heavy alcohol consumption
- Chronic acid reflux (GERD) and Barrett’s esophagus
- Obesity and central weight gain
- Diets low in fruits/vegetables; exposure to very hot beverages
- Older age and male sex (risk increases with age)
- Certain environmental exposures and rare inherited conditions
Having risk factors doesn’t mean you will develop cancer, but discussing them with a clinician can guide screening and prevention.
Diagnosis & Staging
If oesophagus cancer is suspected, your care team may use:
- Upper endoscopy (EGD): camera-guided examination with tissue biopsy
- Imaging: CT, PET/CT, or endoscopic ultrasound (EUS) to assess spread
- Pathology: confirms cancer type and molecular features
Staging (I–IV) reflects tumour depth, lymph node involvement, and metastasis. Accurate staging helps tailor treatment.
Treatment Options
Care plans are individualized by stage, overall health, and cancer type. Treatments may include:
- Surgery: removal of part or most of the esophagus (esophagectomy), sometimes after pre-operative therapy.
- Chemotherapy & Radiation: used before surgery (neoadjuvant), after surgery (adjuvant), or as primary treatment when surgery isn’t possible.
- Immunotherapy: helps the immune system target cancer cells in selected cases.
- Targeted Therapy: aims at specific tumour markers when present.
- Supportive Procedures: stents or feeding tubes to improve swallowing and nutrition.
- Nutrition & Symptom Care: dietitian support, pain control, and rehabilitation are integral to treatment.
Early-stage esophagus cancer generally has more curative options. Advanced stages focus on control of disease and quality of life.
Prevention & Early Detection
Living With Esophagus Cancer
A multidisciplinary team—surgeons, medical and radiation oncologists, gastroenterologists, dietitians, and counsellors—can support you through treatment decisions, side-effect management, nutrition, and emotional wellbeing. Consider joining reputable support groups and ask your care team about rehabilitation and survivorship planning.
FAQs About Esophagus Cancer
Yes. “Esophagus cancer” and “esophageal cancer” are used interchangeably.
There is no single cause. Tobacco, alcohol, chronic reflux, and Barrett’s esophagus are key contributors alongside age and other factors.
Many early-stage cases can be cured. Outcomes depend on stage, overall health, and response to therapy.
There’s no universal screening, but individuals with Barrett’s esophagus or significant risk factors may need regular endoscopic surveillance per a doctor’s guidance.
Side effects vary by therapy and can include fatigue, swallowing changes, taste changes, weight loss, and digestive issues. Your care team will help manage them.


