Weight Loss Surgery: Symptoms, Treatment & Care
What Is Weight Loss Surgery?
Weight loss surgery, also known as bariatric surgery, is a medical procedure that helps people with severe obesity lose weight by altering the digestive system. Obesity is a chronic metabolic condition caused by excess fat accumulation, often measured by Body Mass Index (BMI). When lifestyle changes and medications are not enough, weight loss surgery may be recommended to improve health, reduce obesity-related risks, and enhance quality of life.
Signs & Symptoms of Obesity
Obesity can lead to a variety of symptoms and health challenges, including:
- Excess body fat, especially around the abdomen
- Shortness of breath or difficulty in physical activity
- Joint pain and mobility issues
- Snoring or Sleep apnea
- Persistent fatigue and low energy
- Increased sweating
- Emotional stress, low confidence, or depression
Risk Factors for Obesity
Certain factors increase the risk of obesity and the need for weight loss surgery:
- Genetics and family history
- Sedentary lifestyle and lack of exercise
- High-calorie diet rich in processed or fast food
- Hormonal or metabolic disorders
- Psychological conditions like stress or emotional eating
- Certain medications that promote weight gain
Diagnosis & Staging of Obesity
Doctors assess obesity using:
- Body Mass Index (BMI): A BMI over 30 is classified as obese
- Waist circumference: Higher values indicate abdominal fat risk
- Medical history: Family, lifestyle, and associated health conditions
- Blood tests: To check for diabetes, cholesterol, thyroid, and other metabolic factors
Staging obesity involves assessing its severity and related health risks, such as type 2 diabetes, hypertension, and heart disease.
Treatment Options for Weight Loss
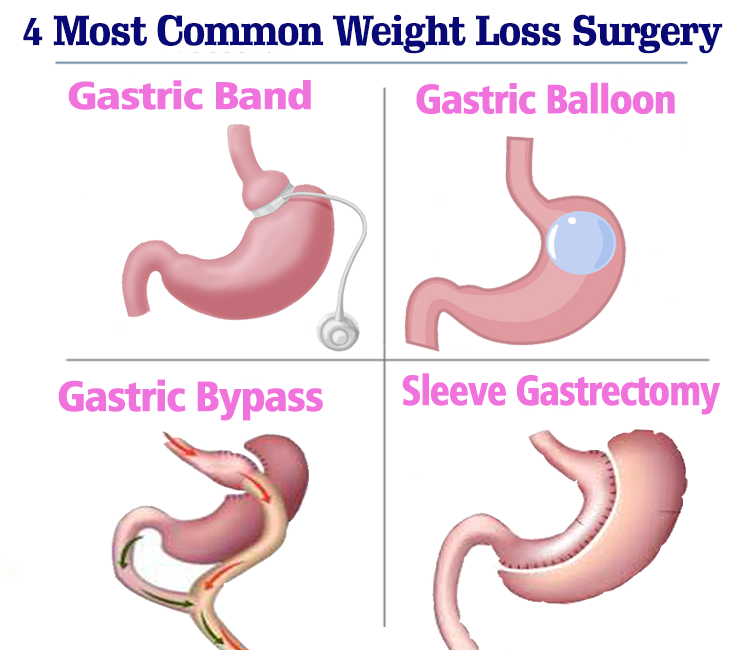
Weight loss surgery is usually recommended for people with a BMI of 40 or higher, or BMI of 35+ with obesity-related health conditions. Common surgical options include:
- Gastric Bypass Surgery: Creates a small stomach pouch and reroutes the digestive tract to limit food absorption
- Sleeve Gastrectomy: Removes part of the stomach, reducing its size and appetite hormones
- Adjustable Gastric Banding: Places a band around the upper stomach to limit food intake
- Biliopancreatic Diversion with Duodenal Switch (BPD/DS): A more complex surgery that reduces stomach size and bypasses a large part of the intestine
Non-surgical treatments may include diet management, exercise, behavior therapy, and medications under medical supervision.
Prevention & Early Detection of Obesity
Obesity can often be prevented or managed through:
FAQs About Weight Loss Surgery
Weight Loss Surgery is usually recommended for individuals with a BMI of 40 or higher, or a BMI of 35 or more with obesity-related health conditions such as type 2 diabetes, heart disease, or sleep apnea.
Yes. Modern Weight Loss Surgery is generally safe, but like all surgical procedures, it carries some risks. Long-term success depends on proper follow-up care, dietary changes, and lifestyle adjustments.
Most patients lose 50–70% of their excess weight within 12–18 months following Weight Loss Surgery. Results vary depending on the procedure type and the patient’s commitment to healthy lifestyle habits.
Yes. Weight regain is possible if lifestyle changes are not maintained. To achieve lasting results, Weight Loss Surgery must be combined with a healthy diet, regular physical activity, and ongoing medical follow-up.
Weight Loss Surgery can significantly improve overall health by reducing or resolving obesity-related conditions such as type 2 diabetes, high blood pressure, sleep apnea, joint pain, and heart disease. It also boosts mobility, energy levels, and self-confidence.


